2022年
No.11
Filters applied: from 2022/11/1 - 2022/11/30.
1. Cell. 2022 Nov 23;185(24):4467-4469. doi: 10.1016/j.cell.2022.10.029.
Need for speed: Key driver of host cell migration varies among mycobacteria.
Youngblom MA(1), Pepperell CS(2).
Author information:
(1)Microbiology Doctoral Training Program, University of Wisconsin-Madison,
Madison, WI, USA; Department of Medical Microbiology and Immunology, School of
Medicine and Public Health, University of Wisconsin-Madison, Madison, WI, USA.
(2)Department of Medical Microbiology and Immunology, School of Medicine and
Public Health, University of Wisconsin-Madison, Madison, WI, USA; Department of
Medicine (Infectious Diseases), School of Medicine and Public Health, University
of Wisconsin-Madison, Madison, WI, USA. Electronic address:
cspepper@medicine.wisc.edu.
In this issue of Cell, Saelens et al. describe a new function for mycobacterial
Type VII secretion systems: manipulation of host cell migration. They find that
a substantial proportion of global TB cases arise from bacteria lacking this
function, raising questions about its role in pathoadaptation of Mycobacterium
tuberculosis.
Copyright © 2022 Elsevier Inc. All rights reserved.
DOI: 10.1016/j.cell.2022.10.029
PMID: 36423577 [Indexed for MEDLINE]
2. Lancet. 2022 Nov 26;400(10366):1858-1868. doi: 10.1016/S0140-6736(22)02078-5.
Epub 2022 Nov 8.
Evaluation of two short standardised regimens for the treatment of
rifampicin-resistant tuberculosis (STREAM stage 2): an open-label, multicentre,
randomised, non-inferiority trial.
Goodall RL(1), Meredith SK(2), Nunn AJ(2), Bayissa A(3), Bhatnagar AK(4),
Bronson G(5), Chiang CY(6), Conradie F(7), Gurumurthy M(8), Kirenga B(9), Kiria
N(10), Meressa D(11), Moodliar R(12), Narendran G(13), Ngubane N(14), Rassool
M(15), Sanders K(2), Solanki R(16), Squire SB(17), Torrea G(18), Tsogt B(19),
Tudor E(20), Van Deun A(18), Rusen ID(5); STREAM study collaborators.
Author information:
(1)Medical Research Council Clinical Trials Unit at UCL, University College
London, London, UK. Electronic address: r.goodall@ucl.ac.uk.
(2)Medical Research Council Clinical Trials Unit at UCL, University College
London, London, UK.
(3)Armauer Hansen Research Institute, Addis Ababa, Ethiopia.
…
Erratum in
Lancet. 2022 Nov 19;400(10365):1766.
Comment in
Lancet. 2022 Nov 26;400(10366):1823-1825.
BACKGROUND: The STREAM stage 1 trial showed that a 9-month regimen for the
treatment of rifampicin-resistant tuberculosis was non-inferior to the 20-month
2011 WHO-recommended regimen. In STREAM stage 2, we aimed to compare two
bedaquiline-containing regimens with the 9-month STREAM stage 1 regimen.
METHODS: We did a randomised, phase 3, non-inferiority trial in 13 hospital
clinics in seven countries, in individuals aged 15 years or older with
rifampicin-resistant tuberculosis without fluoroquinolone or aminoglycoside
resistance. Participants were randomly assigned 1:2:2:2 to the 2011 WHO regimen
(terminated early), a 9-month control regimen, a 9-month oral regimen with
bedaquiline (primary comparison), or a 6-month regimen with bedaquiline and 8
weeks of second-line injectable. Randomisations were stratified by site, HIV
status, and CD4 count. Participants and clinicians were aware of treatment-group
assignments, but laboratory staff were masked. The primary outcome was
favourable status (negative cultures for Mycobacterium tuberculosis without a
preceding unfavourable outcome) at 76 weeks; any death, bacteriological failure
or recurrence, and major treatment change were considered unfavourable outcomes.
All comparisons used groups of participants randomly assigned concurrently. For
non-inferiority to be shown, the upper boundary of the 95% CI should be less
than 10% in both modified intention-to-treat (mITT) and per-protocol analyses,
with prespecified tests for superiority done if non-inferiority was shown. This
trial is registered with ISRCTN, ISRCTN18148631.
FINDINGS: Between March 28, 2016, and Jan 28, 2020, 1436 participants were
screened and 588 were randomly assigned. Of 517 participants in the mITT
population, 133 (71%) of 187 on the control regimen and 162 (83%) of 196 on the
oral regimen had a favourable outcome: a difference of 11·0% (95% CI 2·9-19·0),
adjusted for HIV status and randomisation protocol (p<0·0001 for
non-inferiority). By 76 weeks, 108 (53%) of 202 participants on the control
regimen and 106 (50%) of 211 allocated to the oral regimen had an adverse event
of grade 3 or 4; five (2%) participants on the control regimen and seven (3%) on
the oral regimen had died. Hearing loss (Brock grade 3 or 4) was more frequent
in participants on the control regimen than in those on the oral regimen (18
[9%] vs four [2%], p=0·0015). Of 134 participants in the mITT population who
were allocated to the 6-month regimen, 122 (91%) had a favourable outcome
compared with 87 (69%) of 127 participants randomly assigned concurrently to the
control regimen (adjusted difference 22·2%, 95% CI 13·1-31·2); six (4%) of 143
participants on the 6-month regimen had grade 3 or 4 hearing loss.
INTERPRETATION: Both bedaquiline-containing regimens, a 9-month oral regimen and
a 6-month regimen with 8 weeks of second-line injectable, had superior efficacy
compared with a 9-month injectable-containing regimen, with fewer cases of
hearing loss.
FUNDING: USAID and Janssen Research & Development.
Copyright © 2022 The Author(s). Published by Elsevier Ltd. This is an Open
Access article under the CC BY 4.0 license. Published by Elsevier Ltd.. All
rights reserved.
DOI: 10.1016/S0140-6736(22)02078-5
PMID: 36368336 [Indexed for MEDLINE]
3. Cell. 2022 Nov 23;185(24):4507-4525.e18. doi: 10.1016/j.cell.2022.10.019. Epub
2022 Nov 9.
An ancestral mycobacterial effector promotes dissemination of infection.
Saelens JW(1), Sweeney MI(1), Viswanathan G(1), Xet-Mull AM(1), Jurcic Smith
KL(1), Sisk DM(1), Hu DD(2), Cronin RM(3), Hughes EJ(1), Brewer WJ(1), Coers
J(4), Champion MM(5), Champion PA(6), Lowe CB(1), Smith CM(1), Lee S(7), Stout
JE(8), Tobin DM(9).
Author information:
(1)Department of Molecular Genetics and Microbiology, Duke University School of
Medicine, Durham, NC 27710, USA.
(2)Department of Chemistry and Biochemistry, University of Notre Dame, Notre
Dame, IN 46556, USA.
(3)Department of Biological Sciences, University of Notre Dame, Notre Dame, IN
46556, USA.
…
The human pathogen Mycobacterium tuberculosis typically causes lung disease but
can also disseminate to other tissues. We identified a M. tuberculosis (Mtb)
outbreak presenting with unusually high rates of extrapulmonary dissemination
and bone disease. We found that the causal strain carried an ancestral
full-length version of the type VII-secreted effector EsxM rather than the
truncated version present in other modern Mtb lineages. The ancestral EsxM
variant exacerbated dissemination through enhancement of macrophage motility,
increased egress of macrophages from established granulomas, and alterations in
macrophage actin dynamics. Reconstitution of the ancestral version of EsxM in an
attenuated modern strain of Mtb altered the migratory mode of infected
macrophages, enhancing their motility. In a zebrafish model, full-length EsxM
promoted bone disease. The presence of a derived nonsense variant in EsxM
throughout the major Mtb lineages 2, 3, and 4 is consistent with a role for EsxM
in regulating the extent of dissemination.
Copyright © 2022 The Authors. Published by Elsevier Inc. All rights reserved.
DOI: 10.1016/j.cell.2022.10.019
PMCID: PMC9691622
PMID: 36356582 [Indexed for MEDLINE]
4. Cancer Cell. 2022 Nov 11:S1535-6108(22)00521-9. doi:
10.1016/j.ccell.2022.10.024. Online ahead of print.
Understanding NSCLC, one cell at a time.
Ballesteros I(1), Cerezo-Wallis D(2), Hidalgo A(3).
Author information:
(1)Area of Cell & Developmental Biology, Centro Nacional de Investigaciones
Cardiovasculares Carlos III, Madrid, Spain.
(2)Vascular Biology and Therapeutics Program and Department of Immunobiology,
Yale University School of Medicine, New Haven, CT, USA.
(3)Area of Cell & Developmental Biology, Centro Nacional de Investigaciones
Cardiovasculares Carlos III, Madrid, Spain; Vascular Biology and Therapeutics
Program and Department of Immunobiology, Yale University School of Medicine, New
Haven, CT, USA. Electronic address: ahidalgo@cnic.es.
Lung cancers are very heterogeneous, a feature that in part emanates from the
tumor microenvironment. In this issue, Salcher et al. provide a comprehensive
analysis of hundreds of patients with non-small cell lung cancer (NSCLC) at the
single-cell level to discover extreme immune diversity and define neutrophil
populations associated with treatment outcome.
Copyright © 2022 Elsevier Inc. All rights reserved.
DOI: 10.1016/j.ccell.2022.10.024
PMID: 36400019
5. Nat Med. 2022 Nov;28(11):2353-2363. doi: 10.1038/s41591-022-02047-z. Epub 2022
Nov 10.
Overall survival with circulating tumor DNA-guided therapy in advanced
non-small-cell lung cancer.
Jee J(1), Lebow ES(1), Yeh R(1), Das JP(1), Namakydoust A(1), Paik PK(1)(2),
Chaft JE(1)(2), Jayakumaran G(1), Rose Brannon A(1), Benayed R(1), Zehir A(1),
…
Author information:
(1)Memorial Sloan Kettering Cancer Center, New York, NY, USA.
(2)Weill Cornell Medicine, Cornell University, New York, NY, USA.
(3)Guangdong Lung Cancer Institute, Guangdong Provincial People's Hospital and
Guangdong Academy of Medical Sciences, Guangzhou, China.
…
Comment in
Nat Med. 2022 Nov;28(11):2255-2256.
Circulating tumor DNA (ctDNA) sequencing guides therapy decisions but has been
studied mostly in small cohorts without sufficient follow-up to determine its
influence on overall survival. We prospectively followed an international cohort
of 1,127 patients with non-small-cell lung cancer and ctDNA-guided therapy.
ctDNA detection was associated with shorter survival (hazard ratio (HR), 2.05;
95% confidence interval (CI), 1.74-2.42; P < 0.001) independently of
clinicopathologic features and metabolic tumor volume. Among the 722 (64%)
patients with detectable ctDNA, 255 (23%) matched to targeted therapy by ctDNA
sequencing had longer survival than those not treated with targeted therapy (HR,
0.63; 95% CI, 0.52-0.76; P < 0.001). Genomic alterations in ctDNA not detected
by time-matched tissue sequencing were found in 25% of the patients. These
ctDNA-only alterations disproportionately featured subclonal drivers of
resistance, including RICTOR and PIK3CA alterations, and were associated with
short survival. Minimally invasive ctDNA profiling can identify heterogeneous
drivers not captured in tissue sequencing and expand community access to
life-prolonging therapy.
© 2022. The Author(s), under exclusive licence to Springer Nature America, Inc.
DOI: 10.1038/s41591-022-02047-z
PMID: 36357680 [Indexed for MEDLINE]
6. Cancer Cell. 2022 Nov 14;40(11):1279-1293. doi: 10.1016/j.ccell.2022.09.018.
Epub 2022 Oct 20.
Squamous cell lung cancer: Current landscape and future therapeutic options.
Lau SCM(1), Pan Y(1), Velcheti V(1), Wong KK(2).
Author information:
(1)Department of Medical Oncology, Laura & Issac Perlmutter Cancer Center, NYU
Grossman School of Medicine, NYU Langone Health, Smilow Building 10th Floor,
Suite 1001, New York, NY 10016, USA.
(2)Department of Medical Oncology, Laura & Issac Perlmutter Cancer Center, NYU
Grossman School of Medicine, NYU Langone Health, Smilow Building 10th Floor,
Suite 1001, New York, NY 10016, USA. Electronic address:
kwok-kin.wong@nyulangone.org.
Squamous cell lung cancers (lung squamous cell carcinomas [LUSCs]) are
associated with high mortality and a lack of therapies specific to this disease.
Although recurrent molecular aberrations are present in LUSCs, efforts to
develop targeted therapies against receptor tyrosine kinases, signaling
transduction, and cell cycle checkpoints in LUSCs were met with significant
challenges. The present therapeutic landscape focuses on epigenetic therapies to
modulate the expression of lineage-dependent survival pathways and undruggable
oncogenes. Another important therapeutic approach is to exploit metabolic
vulnerabilities unique to LUSCs. These novel therapies may synergize with immune
checkpoint inhibitors in the right therapeutic context. For example, the
recognition that alterations in KEAP1-NFE2L2 in LUSCs affected antitumor immune
responses created unique opportunities for targeted, metabolic, and immune
combinations. This article provides a perspective on how lessons learned from
the past influence the current therapeutic landscape and opportunities for
future drug development for LUSCs.
Copyright © 2022 Elsevier Inc. All rights reserved.
DOI: 10.1016/j.ccell.2022.09.018
PMID: 36270277 [Indexed for MEDLINE]
7. Lancet Oncol. 2022 Nov;23(11):1465-1474. doi: 10.1016/S1470-2045(22)00600-3.
Epub 2022 Oct 18.
Association of the interaction between mosaic chromosomal alterations and
polygenic risk score with the risk of lung cancer: an array-based case-control
association and prospective cohort study.
Qin N(1), Wang C(2), Chen C(3), Yang L(3), Liu S(3), Xiang J(3), Xie Y(4), Liang
S(3), Zhou J(3), Xu X(3), Zhao X(3), Zhu M(5), Jin G(6), Ma H(7), Dai J(8), Hu
Z(9), Shen H(10).
Author information:
(1)State Key Laboratory of Reproductive Medicine, School of Public Health,
Nanjing Medical University, Nanjing, China; Department of Epidemiology, Centre
for Global Health, School of Public Health, Nanjing Medical University, Nanjing,
China; Jiangsu Key Lab of Cancer Biomarkers, Prevention and Treatment,
Collaborative Innovation Centre for Cancer Medicine, Nanjing Medical University,
Nanjing, China.
(2)Jiangsu Key Lab of Cancer Biomarkers, Prevention and Treatment, Collaborative
Innovation Centre for Cancer Medicine, Nanjing Medical University, Nanjing,
China; Department of Bioinformatics, School of Biomedical Engineering and
Informatics, Nanjing Medical University, Nanjing, China.
(3)Department of Epidemiology, Centre for Global Health, School of Public
Health, Nanjing Medical University, Nanjing, China.
…
BACKGROUND: Mosaic chromosomal alterations (mCAs) detected from blood-derived
DNA are large structural alterations of clonal haematopoietic origin and are
associated with various diseases, such as haematological malignancies,
infections, and solid cancers. We aimed to investigate whether mCAs contribute
to the risk of lung cancer and modify the effect of polygenic risk score (PRS)
on lung cancer risk prediction.
METHODS: The blood-derived DNA of patients with lung cancer and cancer-free
controls with Chinese ancestry from the Nanjing Lung Cancer Cohort (NJLCC) study
were genotyped with a Global Screening Array, and mCAs were detected with the
Mosaic Chromosomal Alterations (MoChA) pipeline. mCA call sets of individuals
with European ancestry were obtained from the prospective cohort UK Biobank
(UKB) study, including documented incident lung cancer. All patients with lung
cancer from the NJLCC study (aged 15 years or older at diagnosis) were
histopathologically confirmed as new lung cancer cases by at least two
pathologists and were free of chemotherapy or radiotherapy before diagnosis.
Participants with incident lung cancer (aged 37-73 years at assessment)
diagnosed after recruitment to the UKB were identified through linkage to
national cancer registries. Logistic regression and Cox proportional hazard
models were applied to evaluate associations between mCAs and risk of lung
cancer in the NJLCC (logistic regression) and UKB (Cox proportional hazard
model) studies.
FINDINGS: The NJLCC study included 10 248 individuals (6445 [62·89%] men and
3803 [37·11%] women; median age 60·0 years [IQR 53·0-66·0]) with lung cancer and 9298
individuals (5871 [63·14%] men and 3427 [36·86%] women; median age 60·0 years [52·0-65·0])
without lung cancer recruited from three sub-regions (north, central, and south) across China
between April 15, 2003, and Aug 18, 2017. The UKB included 450 821 individuals recruited from
22 centres across the UK between March 13, 2006, and Nov 1, 2010, including 2088 individuals
with lung cancer (1075 [51·48%] men and 1013 [48·52%] women; median age 63·0 years [IQR
59·0-66·0]), and 448 733 participants were free of lung cancer (204 713 [45·62%]
men and 244 020 [54·38%] women; median age 58·0 years [IQR 50·0-63·0]). Compared with
non-carriers of mosaic losses, carriers had a significantly increased risk of lung cancer in the
NJLCC (odds ratio [OR] 1·81, 95% CI 1·43-2·28; p=6·69 × 10-7) and UKB (hazard
ratio [HR] 1·40, 95% CI 1·00-1·95; p=0·048) studies. This increased risk was even higher in patients
with expanded cell fractions of mCAs (ie, cell fractions ≥10% vs cell fractions<10%) in the NJLCC
(OR 1·61 [95% CI 1·26-2·08] vs 1·03 [0·83-1·26]; p for heterogeneity test=6·41 × 10-3).
A significant multiplicative interaction was observed between PRS and mosaic losses on the risk of
lung cancer in both the NJLCC (interaction p value=0·030) and UKB (p=0·043). Compared with
non-carriers of mosaic loss abnormalities with low genetic risk, participants with expanded mosaic
losses (cell fractions ≥10%) and high genetic risk had around a six-times increased risk of lung cancer
in the NJLCC study (OR 6·40 [95% CI 3·22-12·69]), and an almost four-times increased risk of lung cancer
(HR 3·75 [95% CI 1·86-7·55]) in the UKB study. The additive interaction also contributed a 3·67 (95% CI 0·49-6·85)
relative excess risk of developing lung cancer in the NJLCC study, and a 2·15 (0·12-4·19) relative excess
risk in the UKB study.
INTERPRETATION: mCAs act as a new endogenous indicator for the risk of lung
cancer and might be jointly used with PRS to optimise personalised risk
stratification for lung cancer.
FUNDING: National Natural Science Foundation of China, Outstanding Youth
Foundation of Jiangsu Province, Natural Science Foundation of Jiangsu Province,
and Postdoctoral Science Foundation of China.
TRANSLATION: For the Chinese translation of the abstract see Supplementary
Materials section.
Copyright © 2022 Elsevier Ltd. All rights reserved.
DOI: 10.1016/S1470-2045(22)00600-3
PMID: 36265503 [Indexed for MEDLINE]
8. Nat Med. 2022 Nov;28(11):2374-2380. doi: 10.1038/s41591-022-01977-y. Epub 2022
Aug 25.
Cemiplimab plus chemotherapy versus chemotherapy alone in non-small cell lung
cancer: a randomized, controlled, double-blind phase 3 trial.
Gogishvili M(1), Melkadze T(2), Makharadze T(3), Giorgadze D(4), Dvorkin M(5),
Penkov K(6), Laktionov K(7), Nemsadze G(8), Nechaeva M(9), Rozhkova I(10),
Kalinka E(11), Gessner C(12)(13), Moreno-Jaime B(14), Passalacqua R(15), Li
S(16), McGuire K(16), Kaul M(16), Paccaly A(16), Quek RGW(16), Gao B(16),
Seebach F(16), Weinreich DM(16), Yancopoulos GD(16), Lowy I(16), Gullo G(16),
Rietschel P(16).
Author information:
(1)High Technology Medical Centre, University Clinic Ltd., Tbilisi, Georgia.
mirandagogishvili@yahoo.com.
(2)Acad. F. Todua Medical Center, Tbilisi, Georgia.
(3)LTD High Technology Hospital Med Center, Batumi, Georgia.
…
First-line cemiplimab (anti-programmed cell death-1 (PD-1)) monotherapy has
previously shown significant improvement in overall survival (OS) and
progression-free survival (PFS) versus chemotherapy in patients with advanced
non-small cell lung cancer (aNSCLC) and PD-ligand 1 (PD-L1) expression ≥50%.
EMPOWER-Lung 3 ( NCT03409614 ), a double-blind, placebo-controlled, phase 3
study, examined cemiplimab plus platinum-doublet chemotherapy as first-line
treatment for aNSCLC, irrespective of PD-L1 expression or histology. In this
study, 466 patients with stage III/IV aNSCLC without EGFR, ALK or ROS1 genomic
tumor aberrations were randomized (2:1) to receive cemiplimab 350 mg (n = 312)
or placebo (n = 154) every 3 weeks for up to 108 weeks in combination with four
cycles of platinum-doublet chemotherapy (followed by pemetrexed maintenance as
indicated). In total, 57.1% (266/466 patients) had non-squamous NSCLC, and 85.2%
(397/466 patients) had stage IV disease. The primary endpoint was OS. The trial
was stopped early per recommendation of the independent data monitoring
committee, based on meeting preset OS efficacy criteria: median OS was
21.9 months (95% confidence interval (CI), 15.5-not evaluable) with cemiplimab
plus chemotherapy versus 13.0 months (95% CI, 11.9-16.1) with placebo plus
chemotherapy (hazard ratio (HR) = 0.71; 95% CI, 0.53-0.93; P = 0.014). Grade ≥3
adverse events occurred with cemiplimab plus chemotherapy (43.6%, 136/312
patients) and placebo plus chemotherapy (31.4%, 48/153 patients). Cemiplimab is
only the second anti-PD-1/PD-L1 agent to show efficacy in aNSCLC as both
monotherapy and in combination with chemotherapy for both squamous and
non-squamous histologies.
© 2022. The Author(s).
DOI: 10.1038/s41591-022-01977-y
PMCID: PMC9671806
PMID: 36008722 [Indexed for MEDLINE]
9. Nat Rev Microbiol. 2022 Nov;20(11):685-701. doi: 10.1038/s41579-022-00731-y.
Epub 2022 Apr 27.
Anti-tuberculosis treatment strategies and drug development: challenges and
priorities.
Dartois VA(1), Rubin EJ(2).
Author information:
(1)Center for Discovery and Innovation, and Hackensack Meridian School of
Medicine, Department of Medical Sciences, Hackensack Meridian Health, Nutley,
NJ, USA. veronique.dartois@hmh-cdi.org.
(2)Harvard T.H. Chan School of Public Health, Department of Immunology and
Infectious Diseases, Boston, MA, USA.
Despite two decades of intensified research to understand and cure tuberculosis
disease, biological uncertainties remain and hamper progress. However, owing to
collaborative initiatives including academia, the pharmaceutical industry and
non-for-profit organizations, the drug candidate pipeline is promising. This
exceptional success comes with the inherent challenge of prioritizing multidrug
regimens for clinical trials and revamping trial designs to accelerate regimen
development and capitalize on drug discovery breakthroughs. Most wanted are
markers of progression from latent infection to active pulmonary disease,
markers of drug response and predictors of relapse, in vitro tools to uncover
synergies that translate clinically and animal models to reliably assess the
treatment shortening potential of new regimens. In this Review, we highlight the
benefits and challenges of 'one-size-fits-all' regimens and treatment duration
versus individualized therapy based on disease severity and host and pathogen
characteristics, considering scientific and operational perspectives.
© 2022. Springer Nature Limited.
DOI: 10.1038/s41579-022-00731-y
PMCID: PMC9045034
PMID: 35478222 [Indexed for MEDLINE]
10. J Natl Cancer Inst. 2022 Nov 29:djac208. doi: 10.1093/jnci/djac208. Online ahead of print.
Association between imaging surveillance frequency and outcomes following
surgical treatment of early-stage lung cancer.
Heiden BT(1), Eaton DB(2), Chang SH(2)(3), Yan Y(2)(3), Schoen MW(2)(4), Thomas
TS(2)(5), Patel MR(2), Kreisel D(1)(2), Nava RG(1)(2), Meyers BF(1), Kozower
BD(1), Puri V(1)(2).
Author information:
(1)Division of Cardiothoracic Surgery, Department of Surgery, Washington
University School of Medicine, St. Louis, MO, USA.
(2)VA St. Louis Health Care System, St. Louis, MO, USA.
(3)Division of Public Health Sciences, Department of Surgery, Washington
University School of Medicine, St. Louis, MO, USA.
(4)Division of Hematology and Medical Oncology, Department of Internal Medicine,
Saint Louis University School of Medicine, St. Louis, MO, USA.
(5)Divisions of Hematology & Oncology, Department of Medicine, Washington
University School of Medicine, St. Louis, MO, USA.
BACKGROUND: Recent studies have suggested that more frequent post-operative
surveillance imaging via computed tomography (CT) following lung cancer
resection may not improve outcomes. We sought to validate these findings using a
uniquely compiled dataset from the Veterans Health Administration, the largest
integrated healthcare system in the United States.
METHODS: We performed a retrospective cohort study of Veterans with pathologic
stage I non-small cell lung cancer (NSCLC) receiving surgery (2006-2016). We
assessed the relationship between surveillance frequency (chest CT scans within
2 years after surgery) and recurrence-free survival and overall survival.
RESULTS: Among 6171 patients, 3047 (49.4%) and 3124 (50.6%) underwent
low-frequency (<2 scans/year; every 6-12 months) and high-frequency (≥2
scans/year; every 3-6 months) surveillance, respectively. Factors associated
with high-frequency surveillance included being a former smoker (vs. current,
adjusted odds ratio [aOR] 1.18, 95% CI 1.05-1.33), receiving a wedge resection
(vs. lobectomy, aOR 1.21, 95% CI 1.05-1.39), and having follow-up with an
oncologist (aOR 1.58, 95% CI 1.42-1.77), whereas African American race was
associated with low-frequency surveillance (vs. White race, aOR 0.64, 95% CI
0.54-0.75). With a median (IQR) follow-up of 7.3 (3.4-12.5) years, recurrence
was detected in 1360 (22.0%) patients. High-frequency surveillance was not
associated with longer recurrence-free survival (adjusted hazard ratio [aHR],
0.93; 95% CI, 0.83-1.04, p = 0.22) or overall survival (aHR, 1.04; 95% CI,
0.96-1.12, p = 0.35).
CONCLUSIONS: We found that high-frequency surveillance does not improve outcomes
in surgically treated stage I NSCLC. Future lung cancer treatment guidelines
should consider less frequent surveillance imaging in patients with stage I
disease.
© The Author(s) 2022. Published by Oxford University Press. All rights reserved.
For permissions, please email: journals.permissions@oup.com.
DOI: 10.1093/jnci/djac208
PMID: 36442509
11. PLoS Biol. 2022 Nov 28;20(11):e3001906. doi: 10.1371/journal.pbio.3001906.
eCollection 2022 Nov.
The Mycobacterium tuberculosis PE15/PPE20 complex transports calcium across the
outer membrane.
Boradia V(1), Frando A(1), Grundner C(1)(2)(3).
Author information:
(1)Center for Global Infectious Disease Research, Seattle Children's Research
Institute, Seattle, Washington, United States of America.
(2)Department of Pediatrics, University of Washington, Seattle, Washington,
United States of America.
(3)Department of Global Health, University of Washington, Seattle, Washington,
United States of America.
The mechanisms by which nutrients traverse the Mycobacterium tuberculosis (Mtb)
outer membrane remain mostly unknown and, in the absence of classical porins,
likely involve specialized transport systems. Calcium ions (Ca2+) are an
important nutrient and serve as a second messenger in eukaryotes, but whether
bacteria have similar Ca2+ signaling systems is not well understood. To
understand the basis for Ca2+ transport and signaling in Mtb, we determined
Mtb's transcriptional response to Ca2+. Overall, only few genes changed
expression, suggesting a limited role of Ca2+ as a transcriptional regulator.
However, 2 of the most strongly down-regulated genes were the pe15 and ppe20
genes that code for members of a large family of proteins that localize to the
outer membrane and comprise many intrinsically disordered proteins. PE15 and
PPE20 formed a complex and PPE20 directly bound Ca2+. Ca2+-associated phenotypes
such as increased ATP consumption and biofilm formation were reversed in a
pe15/ppe20 knockout (KO) strain, suggesting a direct role in Ca2+ homeostasis.
To test whether the PE15/PPE20 complex has a role in Ca2+ transport across the
outer membrane, we created a fluorescence resonance energy transfer (FRET)-based
Ca2+ reporter strain. A pe15/ppe20 KO in the FRET background showed a specific
and selective loss of Ca2+ influx that was dependent on the presence of an
intact outer cell wall. These data show that PE15/PPE20 form a Ca2+-binding
protein complex that selectively imports Ca2+, show a distinct transport
function for an intrinsically disordered protein, and support the emerging idea
of a general family-wide role of PE/PPE proteins as idiosyncratic transporters
across the outer membrane.
Copyright: © 2022 Boradia et al. This is an open access article distributed
under the terms of the Creative Commons Attribution License, which permits
unrestricted use, distribution, and reproduction in any medium, provided the
original author and source are credited.
DOI: 10.1371/journal.pbio.3001906
PMCID: PMC9731449
PMID: 36441815 [Indexed for MEDLINE]
12. J Clin Invest. 2022 Nov 22:e153470. doi: 10.1172/JCI153470. Online ahead of
print.
Oncogenic KRAS signaling drives evasion of innate immune surveillance in lung
adenocarcinoma by activating CD47.
Hu H(1), Cheng R(1), Wang Y(1), Wang X(2), Wu J(1), Kong Y(2), Zhan S(1), Zhou
Z(1), Zhu H(2), Yu R(1), Liang G(1), Wang Q(1), Zhu X(1), Zhang CY(1), Yin R(2),
Yan C(1), Chen X(1).
Author information:
(1)State Key Laboratory of Pharmaceutical Sciences, School of Life Sciences,
Nanjing University, Nanjing, China.
(2)Department of Thoracic Surgery, Jiangsu Cancer Hospital, Nanjing, China.
KRAS is one of the most frequently activated oncogenes in human cancers. While
the role of KRAS mutation in tumorigenesis and tumor maintenance has been
extensively studied, the relationship between KRAS and the tumor immune
microenvironment is not fully understood. Herein, we identified a novel role of
KRAS in driving tumor evasion from innate immune surveillance. In lung
adenocarcinoma patient samples and Kras-driven genetic mouse models of lung
cancer, mutant KRAS activated the expression of cluster of differentiation 47
(CD47), an antiphagocytic signal in cancer cells, leading to decreased
phagocytosis of cancer cells by macrophages. Mechanistically, mutant KRAS
activated PI3K-STAT3 signaling, which restrained miR-34a expression and relieved
the post-transcriptional repression of miR-34a on CD47. In three independent
lung cancer patient cohorts, KRAS mutation status positively correlated with
CD47 expression. Therapeutically, disruption of the KRAS-CD47 signaling axis
with KRAS siRNA, the KRASG12C inhibitor AMG 510 or miR-34a mimic suppressed CD47
expression, enhanced the phagocytic capacity of macrophages and restored innate
immune surveillance. Our results revealed a direct mechanistic link between
active KRAS and innate immune evasion and identified CD47 as a major effector
underlying KRAS-mediated immunosuppressive tumor microenvironment.
DOI: 10.1172/JCI153470
PMID: 36413402
13. Nat Commun. 2022 Nov 18;13(1):7068. doi: 10.1038/s41467-022-34853-x.
A comprehensive update to the Mycobacterium tuberculosis H37Rv reference genome.
Chitale P(1)(2), Lemenze AD(3), Fogarty EC(4)(5), Shah A(1)(6), Grady C(1)(2),
Odom-Mabey AR(7)(8), Johnson WE(1)(2)(9), Yang JH(1)(6), Eren AM(10)(11), Brosch
R(12), Kumar P(1)(2), Alland D(13)(14).
Author information:
(1)Ray V. Lourenco Center for the Study of Emerging and Re-emerging Pathogens,
Rutgers University - New Jersey Medical School, Newark, NJ, USA.
(2)Public Health Research Institute, Rutgers University - New Jersey Medical
School, Newark, NJ, USA.
(3)Department of Pathology, Immunology and Laboratory Medicine, New Jersey
Medical School, Rutgers-The State University of New Jersey, Newark, NJ, USA.
…
Erratum in
Nat Commun. 2022 Dec 7;13(1):7538.
H37Rv is the most widely used Mycobacterium tuberculosis strain, and its genome
is globally used as the M. tuberculosis reference sequence. Here, we present
Bact-Builder, a pipeline that uses consensus building to generate complete and
accurate bacterial genome sequences and apply it to three independently cultured
and sequenced H37Rv aliquots of a single laboratory stock. Two of the 4,417,942
base-pair long H37Rv assemblies are 100% identical, with the third differing by
a single nucleotide. Compared to the existing H37Rv reference, the new sequence
contains ~6.4 kb additional base pairs, encoding ten new regions that include
insertions in PE/PPE genes and new paralogs of esxN and esxJ, which are
differentially expressed compared to the reference genes. New sequencing and de
novo assemblies with Bact-Builder confirm that all 10 regions, plus small
additional polymorphisms, are also present in the commonly used H37Rv strains
NR123, TMC102, and H37Rv1998. Thus, Bact-Builder shows promise as an improved
method to perform accurate and reproducible de novo assemblies of bacterial
genomes, and our work provides important updates to the primary M. tuberculosis
reference genome.
© 2022. The Author(s).
DOI: 10.1038/s41467-022-34853-x
PMCID: PMC9673877
PMID: 36400796 [Indexed for MEDLINE]
14. Lancet Infect Dis. 2022 Nov 14:S1473-3099(22)00668-5. doi:
10.1016/S1473-3099(22)00668-5. Online ahead of print.
Effect of systematic tuberculosis detection on mortality in young children with
severe pneumonia in countries with high incidence of tuberculosis: a
stepped-wedge cluster-randomised trial.
Marcy O(1), Wobudeya E(2), Font H(3), Vessière A(3), Chabala C(4), Khosa C(5),
Taguebue JV(6), Moh R(7), Mwanga-Amumpaire J(8), Lounnas M(9), Mulenga V(4),
…
Author information:
(1)Inserm UMR 1219, IRD EMR 271, University of Bordeaux, Bordeaux, France.
Electronic address: olivier.marcy@u-bordeaux.fr.
(2)Makerere University-Johns Hopkins University Research Collaboration, Kampala,
Uganda.
(3)Inserm UMR 1219, IRD EMR 271, University of Bordeaux, Bordeaux, France.
…
BACKGROUND: Tuberculosis diagnosis might be delayed or missed in children with
severe pneumonia because this diagnosis is usually only considered in cases of
prolonged symptoms or antibiotic failure. Systematic tuberculosis detection at
hospital admission could increase case detection and reduce mortality.
METHODS: We did a stepped-wedge cluster-randomised trial in 16 hospitals from
six countries (Cambodia, Cameroon, Côte d'Ivoire, Mozambique, Uganda, and
Zambia) with high incidence of tuberculosis. Children younger than 5 years with
WHO-defined severe pneumonia received either the standard of care (control
group) or standard of care plus Xpert MTB/RIF Ultra (Xpert Ultra; Cepheid,
Sunnyvale, CA, USA) on nasopharyngeal aspirate and stool samples (intervention
group). Clusters (hospitals) were progressively switched from control to
intervention at 5-week intervals, using a computer-generated random sequence,
stratified on incidence rate of tuberculosis at country level, and masked to
teams until 5 weeks before switch. We assessed the effect of the intervention on
primary (12-week all-cause mortality) and secondary (including tuberculosis
diagnosis) outcomes, using generalised linear mixed models. The primary analysis
was by intention to treat. We described outcomes in children with severe acute
malnutrition in a post hoc analysis. This study is registered with
ClinicalTrials.gov (NCT03831906) and the Pan African Clinical Trial Registry
(PACTR202101615120643).
FINDINGS: From March 21, 2019, to March 30, 2021, we enrolled 1401 children in
the control group and 1169 children in the intervention group. In the
intervention group, 1140 (97·5%) children had nasopharyngeal aspirates and 942
(80·6%) had their stool collected; 24 (2·1%) had positive Xpert Ultra. At 12
weeks, 110 (7·9%) children in the control group and 91 (7·8%) children in the
intervention group had died (adjusted odds ratio [OR] 0·986, 95% CI 0·597-1·630, p=0·957),
and 74 (5·3%) children in the control group and 88 (7·5%) children in the intervention group
had tuberculosis diagnosed (adjusted OR 1·238, 95% CI 0·696-2·202, p=0·467).
In children with severe acute malnutrition, 57 (23·8%) of 240 children in the control group
and 53 (17·8%) of 297 children in the intervention group died, and 36 (15·0%) of 240 children
in the control group and 56 (18·9%) of 297 children in the intervention group were diagnosed with
tuberculosis. The main adverse events associated with nasopharyngeal aspirates
were samples with blood in 312 (27·3%) of 1147 children with nasopharyngeal
aspirates attempted, dyspnoea or SpO2 less than 95% in 134 (11·4%) of children,
and transient respiratory distress or SpO2 less than 90% in 59 (5·2%) children.
There was no serious adverse event related to nasopharyngeal aspirates reported
during the trial.
INTERPRETATION: Systematic molecular tuberculosis detection at hospital
admission did not reduce mortality in children with severe pneumonia. High
treatment and microbiological confirmation rates support more systematic use of
Xpert Ultra in this group, notably in children with severe acute malnutrition.
FUNDING: Unitaid and L'Initiative.
TRANSLATION: For the French translation of the abstract see Supplementary
Materials section.
Copyright © 2022 Elsevier Ltd. All rights reserved.
DOI: 10.1016/S1473-3099(22)00668-5
PMID: 36395782
15. J Clin Invest. 2022 Nov 15;132(22):e161308. doi: 10.1172/JCI161308.
BCL6 is regulated by the MAPK/ELK1 axis and promotes KRAS-driven lung cancer.
Li K(1)(2)(3), Liu Y(1), Ding Y(1), Zhang Z(1), Feng J(1), Hu J(1), Chen J(1),
Lian Z(1), Chen Y(4), Hu K(3), Chen Z(5), Cai Z(4), Liu M(1), Pang X(1).
Author information:
(1)Changning Maternity and Infant Health Hospital and Shanghai Key Laboratory of
Regulatory Biology and School of Life Sciences and.
(2)Joint Translational Science and Technology Research Institute, East China
Normal University, Shanghai, China.
(3)Cancer Institute, Fudan University Shanghai Cancer Center, Department of
Oncology, Shanghai Medical College, Fudan University, Shanghai, China.
(4)Department of Biochemistry and Molecular Biology, School of Medicine, Tongji
University, Shanghai, China.
(5)Medical Research Institute, Wuhan University, Wuhan, China.
Mutational activation of KRAS is a common oncogenic event in lung cancer, yet
effective therapies are still lacking. Here, we identify B cell lymphoma 6
(BCL6) as a lynchpin in KRAS-driven lung cancer. BCL6 expression was increased
upon KRAS activation in lung tumor tissue in mice and was positively correlated
with the expression of KRAS-GTP, the active form of KRAS, in various human
cancer cell lines. Moreover, BCL6 was highly expressed in human KRAS-mutant lung
adenocarcinomas and was associated with poor patient survival. Mechanistically,
the MAPK/ERK/ELK1 signaling axis downstream of mutant KRAS directly regulated
BCL6 expression. BCL6 maintained the global expression of prereplication complex
components; therefore, BCL6 inhibition induced stalling of the replication fork,
leading to DNA damage and growth arrest in KRAS-mutant lung cancer cells.
Importantly, BCL6-specific knockout in lungs significantly reduced the tumor
burden and mortality in the LSL-KrasG12D/+ lung cancer mouse model. Likewise,
pharmacological inhibition of BCL6 significantly impeded the growth of
KRAS-mutant lung cancer cells both in vitro and in vivo. In summary, our
findings reveal a crucial role of BCL6 in promoting KRAS-addicted lung cancer
and suggest BCL6 as a therapeutic target for the treatment of this intractable
disease.
DOI: 10.1172/JCI161308
PMCID: PMC9663163
PMID: 36377663 [Indexed for MEDLINE]
16. Nat Commun. 2022 Nov 14;13(1):6944. doi: 10.1038/s41467-022-34627-5.
A fluorogenic probe for predicting treatment response in non-small cell lung
cancer with EGFR-activating mutations.
Deng H(#)(1)(2)(3), Lei Q(#)(4)(5)(6), Wang C(#)(4), Wang Z(4)(6), Chen H(5)(6),
Wang G(5), Yang N(5), Huang D(7), Yu Q(5), Yao M(6), Xiao X(6), Zhu G(6), Cheng
C(6), Li Y(6), Li F(7), Tian P(8), Li W(9)(10)(11).
Author information:
(1)Department of Respiratory and Critical Care Medicine, West China Hospital,
Sichuan University, Chengdu, Sichuan, China. huideng0923@hotmail.com.
(2)Targeted Tracer Research and Development Laboratory, Precision Medicine Key
Laboratory of Sichuan Province, Precision Medicine Research Center, West China
Hospital, Sichuan University, Chengdu, Sichuan, China. huideng0923@hotmail.com.
(3)Institute of Respiratory Health, Frontiers Science Center for Disease-related
Molecular Network, West China Hospital, Sichuan University, Chengdu, Sichuan,
China. huideng0923@hotmail.com.
…
Therapeutic responses of non-small cell lung cancer (NSCLC) to epidermal growth
factor receptor (EGFR) - tyrosine kinase inhibitors (TKIs) are known to be
associated with EGFR mutations. However, a proportion of NSCLCs carrying EGFR
mutations still progress on EGFR-TKI underlining the imperfect correlation.
Structure-function-based approaches have recently been reported to perform
better in retrospectively predicting patient outcomes following EGFR-TKI
treatment than exon-based method. Here, we develop a multicolor
fluorescence-activated cell sorting (FACS) with an EGFR-TKI-based fluorogenic
probe (HX103) to profile active-EGFR in tumors. HX103-based FACS shows an
overall agreement with gene mutations of 82.6%, sensitivity of 81.8% and
specificity of 83.3% for discriminating EGFR-activating mutations from wild-type
in surgical specimens from NSCLC patients. We then translate HX103 to the
clinical studies for prediction of EGFR-TKI sensitivity. When integrating
computed tomography imaging with HX103-based FACS, we find a high correlation
between EGFR-TKI therapy response and probe labeling. These studies demonstrate
HX103-based FACS provides a high predictive performance for response to
EGFR-TKI, suggesting the potential utility of an EGFR-TKI-based probe in
precision medicine trials to stratify NSCLC patients for EGFR-TKI treatment.
© 2022. The Author(s).
DOI: 10.1038/s41467-022-34627-5
PMCID: PMC9663578
PMID: 36376325 [Indexed for MEDLINE]
17. Am J Respir Crit Care Med. 2022 Nov 8. doi: 10.1164/rccm.202109-2019OC. Online ahead of print.
Multi-Dimensional Cell-free DNA Fragmentomic Assay for Detection of Early-Stage
Lung Cancer.
Wang S(1), Meng F(2), Li M(1), Bao H(3), Chen X(4), Zhu M(2), Liu R(4), Xu X(4),
Yang S(4), Wu X(5), Shao Y(6), Xu L(7), Yin R(8).
Author information:
(1)Jiangsu Cancer Institute and Hospital, 26481, Nanjing, Jiangsu, China.
(2)Nanjing Medical University, Nanjing, China.
(3)Geneseeq Tech Inc, Nanjing, China.
(4)Geneseeq Research Institute, Nanjing Geneseeq Technology Inc., Nanjing,
China.
(5)Geneseeq Technology Inc., R&D, Toronto, Ontario, Canada.
(6)Geneseeq Technology Inc., Translational Medicine Research Institute, Toronto,
Ontario, Canada.
(7)Jiangsu Key Laboratory of Molecular and Translational Cancer Research,
Jiangsu Cancer Hospital, Jiangsu Institute of Cancer Research, The Affiliated
Cancer Hospital of Nanjing Medical University, Nanjing, China.
(8)Jiangsu Cancer Hospital, 26481, Nanjing, China; rong_yin@njmu.edu.cn.
RATIONALE: Cell-free DNA (cfDNA) analysis holds promise for early detection of
lung cancer and benefits patients with higher survival. However, the detection
sensitivity of previous cfDNA-based studies was still low to suffice the
clinical use, especially for early-stage tumors.
OBJECTIVES: Establish an accurate and affordable approach for early-stage lung
cancer detection by integrating cfDNA fragmentomics and machine learning models.
METHODS: This study included 350 non-cancer and 432 cancer participants. The
participants' plasma cfDNA samples were profiled by whole-genome sequencing.
Multiple cfDNA features and machine learning models were compared in the
training cohort to achieve an optimal model. Model performance was evaluated in
three validation cohorts.
MEASUREMENTS AND MAIN RESULTS: A stacked ensemble model integrating five cfDNA
features and five machine learning algorithms constructed in the training cohort
(cancer: 113, healthy: 113) outperformed all the models built on individual
feature-algorithm combinations. This integrated model yielded superior
sensitivities of 91.4% at 95.7% specificity for Cohort Validation I [Area Under
the Curve (AUC): 0.984], 84.7% at 98.6% specificity for Validation II (AUC:
0.987), and 92.5% at 94.2% specificity for Additional Validation (AUC: 0.974),
respectively. The model's high performance remained consistent when sequencing
depth was down to 0.5× (AUC: 0.966-0.971). Furthermore, our model is sensitive
to identifying early pathological features (83.2% sensitivity for stage I, 85.0%
sensitivity for<1cm tumor at the 0.66 cutoff).
CONCLUSIONS: We have established a stacked ensemble model using cfDNA
fragmentomics features and achieved superior sensitivity for detecting
early-stage lung cancer, which could promote early diagnosis and benefit more
patients. This article is open access and distributed under the terms of the
Creative Commons Attribution Non-Commercial No Derivatives License 4.0
(http://creativecommons.org/licenses/by-nc-nd/4.0/).
DOI: 10.1164/rccm.202109-2019OC
PMID: 36346614
18. J Natl Cancer Inst. 2022 Nov 8:djac203. doi: 10.1093/jnci/djac203. Online ahead of print.
Disparity in checkpoint inhibitor utilization among commercially insured adult
patients with metastatic lung cancer.
Li M(1), Liao K(1), Chen AJ(2), Cascone T(3), Shen Y(4), Lu Q(5), Shih YT(1).
Author information:
(1)Section of Cancer Economics and Policy, Department of Health Services
Research, University of Texas MD Anderson Cancer Center, Houston, USA.
(2)Sol Price School of Public Policy, University of Southern California, Los
Angeles, USA.
(3)Department of Thoracic/Head and Neck Medical Oncology, University of Texas MD
Anderson Cancer Center, Houston, USA.
(4)Department of Biostatistics, University of Texas MD Anderson Cancer Center,
Houston, USA.
(5)Department of Health Disparities Research, University of Texas MD Anderson
Cancer Center, Houston, USA.
BACKGROUND: There is a lack of evidence from nationwide sample on the disparity
of initiating immune checkpoint inhibitors (ICIs) after metastatic lung cancer
diagnosis.
METHODS: We identified metastatic lung cancer patients diagnosed between 2015
and 2020 from a large nationwide commercial claims database. We analyzed the
time from metastatic lung cancer diagnosis to ICI therapy using Cox proportional
hazard models. Independent variables included county-level measures (quintiles
of percentage of racialized population, quintiles of percentage of population
below poverty, urbanity, and density of medical oncologists) and patient
characteristics (age, sex, Charlson comorbidity index, Medicare Advantage, and
year of diagnosis). All tests were two-sided.
RESULTS: A total of 17,022 patients were included. Counties with a larger
proportion of racialized population appeared to be more urban, have a greater
percentage of its residents in poverty, and have a higher density of medical
oncologists. In Cox analysis, the adjusted hazard ratio of the second, third,
fourth, and highest quintile of percentage of racialized population were 0.89
(95% confidence interval [CI]: 0.82-0.98), 0.85 (95% CI: 0.78-0.93), 0.78 (95%
CI: 0.71-0.86), and 0.71 (95% CI: 0.62-0.81), respectively, compared to counties
in the lowest quintile. The slower ICI therapy initiation was driven by counties
with the highest percentage of Hispanic population and other non-Black
racialized groups.
CONCLUSIONS: Commercially insured patients with metastatic lung cancer who lived
in counties with greater percentage of racialized population had slower
initiation of ICI therapy after lung cancer diagnosis, despite greater density
of oncologists in their neighborhood.
© The Author(s) 2022. Published by Oxford University Press. All rights reserved.
For permissions, please email: journals.permissions@oup.com.
DOI: 10.1093/jnci/djac203
PMID: 36346180
19. Nat Commun. 2022 Nov 4;13(1):6623. doi: 10.1038/s41467-022-34428-w.
Tumor factors stimulate lysosomal degradation of tumor antigens and undermine
their cross-presentation in lung cancer.
Lu Z(#)(1), Chen J(#)(1), Yu P(#)(1), Atherton MJ(2), Gui J(1), Tomar VS(1),
Middleton JD(3), Sullivan NT(4), Singhal S(4), George SS(5), Woolfork AG(6),
Weljie AM(6), Hai T(3), Eruslanov EB(4), Fuchs SY(7).
Author information:
(1)Department of Biomedical Sciences, School of Veterinary Medicine, University
of Pennsylvania, Philadelphia, PA, 19104, USA.
(2)Department of Clinical Sciences & Advanced Medicine, School of Veterinary
Medicine, University of Pennsylvania, Philadelphia, PA, 19104, USA.
(3)Department of Biological Chemistry and Pharmacology, The Ohio State
University, Columbus, OH, 43210, USA.
…
Activities of dendritic cells (DCs) that present tumor antigens are often
suppressed in tumors. Here we report that this suppression is induced by tumor
microenvironment-derived factors, which activate the activating transcription
factor-3 (ATF3) transcription factor and downregulate cholesterol 25-hydroxylase
(CH25H). Loss of CH25H in antigen presenting cells isolated from human lung
tumors is associated with tumor growth and lung cancer progression. Accordingly,
mice lacking CH25H in DCs exhibit an accelerated tumor growth, decreased
infiltration and impaired activation of intratumoral CD8+ T cells. These mice do
not establish measurable long-term immunity against malignant cells that undergo
chemotherapy-induced immunogenic cell death. Mechanistically, downregulation of
CH25H stimulates membrane fusion between endo-phagosomes and lysosomes,
accelerates lysosomal degradation and restricts cross-presentation of tumor
antigens in the intratumoral DCs. Administration of STING agonist MSA-2 reduces
the lysosomal activity in DCs, restores antigen cross presentation, and
increases therapeutic efficacy of PD-1 blockade against tumour challenge in a
CH25H-dependent manner. These studies highlight the importance of downregulation
of CH25H in DCs for tumor immune evasion and resistance to therapy.
© 2022. The Author(s).
DOI: 10.1038/s41467-022-34428-w
PMCID: PMC9636202
PMID: 36333297 [Indexed for MEDLINE]
20. Nat Commun. 2022 Nov 3;13(1):6594. doi: 10.1038/s41467-022-34061-7.
Inflammation and immune activation are associated with risk of Mycobacterium
tuberculosis infection in BCG-vaccinated infants.
Satti I(1), Wittenberg RE(#)(1), Li S(#)(1), Harris SA(1), Tanner R(1), Cizmeci
D(1), Jacobs A(1)(2), Williams N(3), Mulenga H(4), Fletcher HA(5), Scriba TJ(4),
Tameris M(4), Hatherill M(4), McShane H(6).
Author information:
(1)Jenner Institute, Nuffield Department of Medicine, University of Oxford,
Oxford, OX3 7DQ, UK.
(2)Wellcome Centre for Infectious Diseases Research in Africa, University of
Cape Town, Observatory, Cape Town, South Africa.
(3)Nuffield Department of Primary Care Health Sciences, University of Oxford,
Radcliffe Observatory Quarter, Woodstock Road, Oxford, OX2 6GG, UK.
…
Tuberculosis vaccine development is hindered by the lack of validated immune
correlates of protection. Exploring immune correlates of risk of disease and/or
infection in prospective samples can inform this field. We investigate whether
previously identified immune correlates of risk of TB disease also associate
with increased risk of M.tb infection in BCG-vaccinated South African infants,
who became infected with M.tb during 2-3 years of follow-up. M.tb infection is
defined by conversion to positive reactivity in the QuantiFERON test. We
demonstrate that inflammation and immune activation are associated with risk of
M.tb infection. Ag85A-specific IgG is elevated in infants that were subsequently
infected with M.tb, and this is coupled with upregulated gene expression of
immunoglobulin-associated genes and type-I interferon. Plasma levels of
IFN-[Formula: see text]2, TNF-[Formula: see text], CXCL10 (IP-10) and complement
C2 are also higher in infants that were subsequently infected with M.tb.
© 2022. The Author(s).
DOI: 10.1038/s41467-022-34061-7
PMCID: PMC9632577
PMID: 36329009 [Indexed for MEDLINE]
21. J Clin Oncol. 2022 Nov 3:JCO2200975. doi: 10.1200/JCO.22.00975. Online ahead of print.
Durvalumab With or Without Tremelimumab in Combination With Chemotherapy as
First-Line Therapy for Metastatic Non-Small-Cell Lung Cancer: The Phase III
POSEIDON Study.
Johnson ML(1), Cho BC(2), Luft A(3), Alatorre-Alexander J(4), Geater SL(5),
Laktionov K(6), Kim SW(7), Ursol G(8), Hussein M(9), Lim FL(10), Yang CT(11),
Araujo LH(12), Saito H(13), Reinmuth N(14), Shi X(15), Poole L(16), Peters
S(17), Garon EB(18), Mok T(19); POSEIDON investigators.
Author information:
(1)Sarah Cannon Research Institute, Tennessee Oncology, PLLC, Nashville, TN.
(2)Yonsei Cancer Center, Seoul, South Korea.
(3)Leningrad Regional Clinical Hospital, St Petersburg, Russia.
…
PURPOSE: The open-label, phase III POSEIDON study evaluated tremelimumab plus
durvalumab and chemotherapy (T + D + CT) and durvalumab plus chemotherapy (D +
CT) versus chemotherapy alone (CT) in first-line metastatic non-small-cell lung
cancer (mNSCLC).
METHODS: Patients (n = 1,013) with EGFR/ALK wild-type mNSCLC were randomly
assigned (1:1:1) to tremelimumab 75 mg plus durvalumab 1,500 mg and
platinum-based chemotherapy for up to four 21-day cycles, followed by durvalumab
once every 4 weeks until progression and one additional tremelimumab dose;
durvalumab plus chemotherapy for up to four 21-day cycles, followed by
durvalumab once every 4 weeks until progression; or chemotherapy for up to six
21-day cycles (with or without maintenance pemetrexed; all arms). Primary end
points were progression-free survival (PFS) and overall survival (OS) for D + CT
versus CT. Key alpha-controlled secondary end points were PFS and OS for T + D +
CT versus CT.
RESULTS: PFS was significantly improved with D + CT versus CT (hazard ratio
[HR], 0.74; 95% CI, 0.62 to 0.89; P = .0009; median, 5.5 v 4.8 months); a trend
for improved OS did not reach statistical significance (HR, 0.86; 95% CI, 0.72
to 1.02; P = .0758; median, 13.3 v 11.7 months; 24-month OS, 29.6% v 22.1%). PFS
(HR, 0.72; 95% CI, 0.60 to 0.86; P = .0003; median, 6.2 v 4.8 months) and OS
(HR, 0.77; 95% CI, 0.65 to 0.92; P = .0030; median, 14.0 v 11.7 months; 24-month
OS, 32.9% v 22.1%) were significantly improved with T + D + CT versus CT.
Treatment-related adverse events were maximum grade 3/4 in 51.8%, 44.6%, and
44.4% of patients receiving T + D + CT, D + CT, and CT, respectively; 15.5%,
14.1%, and 9.9%, respectively, discontinued treatment because of
treatment-related adverse events.
CONCLUSION: D + CT significantly improved PFS versus CT. A limited course of
tremelimumab added to durvalumab and chemotherapy significantly improved OS and
PFS versus CT, without meaningful additional tolerability burden, representing a
potential new option in first-line mNSCLC.
DOI: 10.1200/JCO.22.00975
PMID: 36327426
22. J Exp Med. 2023 Jan 2;220(1):e20220484. doi: 10.1084/jem.20220484. Epub 2022 Nov 3.
Inherited human ITK deficiency impairs IFN-γ immunity and underlies tuberculosis.
Ogishi M(1)(2), Yang R(#)(1), Rodriguez R(#)(3)(4), Golec DP(#)(5), Martin
E(3)(4), Philippot Q(4)(6), Bohlen J(4)(6), Pelham SJ(1), Arias AA(1)(7)(8),
Khan T(9), Ata M(9), Al Ali F(9), Rozenberg F(10), Kong XF(1), Chrabieh M(4)(6),
…
Author information:
(1)St. Giles Laboratory of Human Genetics of Infectious Diseases, Rockefeller
Branch, Rockefeller University, New York, NY.
(2)The David Rockefeller Graduate Program, Rockefeller University, New York, NY.
(3)Laboratory of Lymphocyte Activation and Susceptibility to EBV Infection,
INSERM UMR1163, Paris, France.
…
Inborn errors of IFN-γ immunity can underlie tuberculosis (TB). We report three
patients from two kindreds without EBV viremia or disease but with severe TB and
inherited complete ITK deficiency, a condition associated with severe EBV
disease that renders immunological studies challenging. They have CD4+ αβ T
lymphocytopenia with a concomitant expansion of CD4-CD8- double-negative (DN) αβ and Vδ2- γδ T
lymphocytes, both displaying a unique CD38+CD45RA+T-bet+EOMES- phenotype. Itk-deficient mice
recapitulated an expansion of the γδ T and DN αβ T lymphocyte populations in the thymus and spleen,
respectively. Moreover, the patients' T lymphocytes secrete small amounts of IFN-γ in response to
TCR crosslinking, mitogens, or forced synapse formation with autologous B
lymphocytes. Finally, the patients' total lymphocytes secrete small amounts of
IFN-γ, and CD4+, CD8+, DN αβ T, Vδ2+ γδ T, and MAIT cells display impaired IFN-γ production
in response to BCG. Inherited ITK deficiency undermines the
development and function of various IFN-γ-producing T cell subsets, thereby
underlying TB.
© 2022 Ogishi et al.
DOI: 10.1084/jem.20220484
PMCID: PMC9641312
PMID: 36326697 [Indexed for MEDLINE]
23. J Natl Cancer Inst. 2022 Nov 2:djac205. doi: 10.1093/jnci/djac205. Online ahead of print.
Predictors of Survival to Immunotherapy and Chemoimmunotherapy in Non-Small Cell
Lung Cancer: A Meta-Analysis.
Di Federico A(1)(2), De Giglio A(1)(2), Gelsomino F(1)(2), Sperandi F(1),
Melotti B(1), Ardizzoni A(1)(2).
Author information:
(1)Medical Oncology, IRCCS Azienda Ospedaliero-Universitaria di Bologna,
Bologna, Italy.
(2)Department of Experimental, Diagnostic and Specialty Medicine (DIMES),
University of Bologna, Bologna, Italy.
BACKGROUND: many patients with non-small cell lung cancer (NSCLC) derive poor
benefit from immunotherapy (IO). For some of them, adding chemotherapy (CT) can
improve the outcomes, but the reliability of PD-L1 expression as the only
biomarker to distinguish these patients is unsatisfactory. We sought to detect
clinicopathological and molecular predictive factors of survival that might be
added to PD-L1 expression in the selection of patients that should receive IO
alone or chemoimmunotherapy (CIT).
METHODS: We conducted a systematic search of randomized controlled clinical
trials (RCT) investigating IO, alone or plus CT, versus CT alone in
treatment-naïve advanced NSCLC patients. Meta-analyses and meta-regression
analyses were performed to investigate IO alone versus CT, CIT versus CT, and IO
alone versus CIT.
RESULTS: 14367 patients with advanced NSCLC across 25 RCT were included.
Squamous histology, male sex, current/former smoker status, PD-L1 expression
≥50%, and high tumor mutational burden (TMB) correlated with improved survival
with IO alone compared to CT. Conversely, female sex, no smoking history,
negative PD-L1 expression, and low TMB correlated with unsatisfactory outcomes
with IO alone versus CT, but not with CIT versus CT. CIT improved survival
versus IO alone in female patients, never smokers, in those having a PD-L1
expression ≥1% (but not with PD-L1 ≥50%) or a low TMB, and in patients with
central nervous system metastasis.
CONCLUSION: these findings suggest some clinicopathological and molecular
features that, added to PD-L1 expression, could help in the selection of the
most appropriate first-line IO-based treatment for advanced NSCLC patients.
© The Author(s) 2022. Published by Oxford University Press.
DOI: 10.1093/jnci/djac205
PMID: 36322815
24. J Clin Invest. 2022 Nov 1;132(21):e157873. doi: 10.1172/JCI157873.
Stromal structure remodeling by B lymphocytes limits T cell activation in lymph
nodes of Mycobacterium tuberculosis-infected mice.
Daniel L(1)(2)(3), Bhattacharyya ND(1)(2)(3), Counoupas C(2)(3)(4), Cai Y(5),
Chen X(5), Triccas JA(2)(3)(4)(6), Britton WJ(2)(6)(7), Feng CG(1)(2)(3)(6).
Author information:
(1)Immunology and Host Defence Group, School of Medical Sciences, Faculty of
Medicine and Health.
(2)Centenary Institute.
(3)Charles Perkins Centre, and.
…
An effective adaptive immune response depends on the organized architecture of
secondary lymphoid organs, including the lymph nodes (LNs). While the cellular
composition and microanatomy of LNs under steady state are well defined, the
impact of chronic tissue inflammation on the structure and function of draining
LNs is incompletely understood. Here we showed that Mycobacterium tuberculosis
infection remodeled LN architecture by increasing the number and paracortical
translocation of B cells. The formation of paracortical B lymphocyte and CD35+
follicular dendritic cell clusters dispersed CCL21-producing fibroblastic
reticular cells and segregated pathogen-containing myeloid cells from
antigen-specific CD4+ T cells. Depletion of B cells restored the chemokine and
lymphoid structure and reduced bacterial burdens in LNs of the chronically
infected mice. Importantly, this remodeling process impaired activation of naive
CD4+ T cells in response to mycobacterial and unrelated antigens during chronic
tuberculosis infection. Our studies reveal a mechanism in the regulation of LN
microanatomy during inflammation and identify B cells as a critical element
limiting the T cell response to persistent intracellular infection in LNs.
DOI: 10.1172/JCI157873
PMCID: PMC9621141
PMID: 36317628 [Indexed for MEDLINE]
25. Ann Intern Med. 2022 Nov;175(11):1501-1505. doi: 10.7326/M22-1325. Epub 2022 Oct 11.
Characteristics of Persons Screened for Lung Cancer in the United States : A
Cohort Study.
Silvestri GA(1), Goldman L(2), Burleson J(2), Gould M(3), Kazerooni EA(4),
Mazzone PJ(5), Rivera MP(6), Doria-Rose VP(7), Rosenthal LS(8), Simanowith M(2),
Smith RA(8), Tanner NT(1), Fedewa S(9).
Author information:
(1)Division of Pulmonary Medicine, Thoracic Oncology Research Group, Hollings
Cancer Center, Medical University of South Carolina, Charleston, South Carolina
(G.A.S., N.T.T.).
(2)American College of Radiology, Reston, Virginia (L.G., J.B., M.S.).
(3)Department of Health Systems Science, Kaiser Permanente Bernard J. Tyson
School of Medicine, Pasadena, California (M.G.).
…
Comment in
Ann Intern Med. 2022 Nov;175(11):1608-1609.
BACKGROUND: Lung cancer screening (LCS) with low-dose computed tomography (LDCT)
was recommended by the U.S. Preventive Services Task Force (USPSTF) in 2013,
making approximately 8 million Americans eligible for screening. The demographic
characteristics and adherence of persons screened in the United States have not
been reported at the population level.
OBJECTIVE: To define sociodemographic characteristics and adherence among
persons screened and entered into the American College of Radiology's Lung
Cancer Screening Registry (LCSR).
DESIGN: Cohort study.
SETTING: United States, 2015 to 2019.
PARTICIPANTS: Persons receiving a baseline LDCT for LCS from 3625 facilities
reporting to the LCSR.
MEASUREMENTS: Age, sex, and smoking status distributions (percentages) were
computed among persons who were screened and among respondents in the 2015
National Health Interview Survey (NHIS) who were eligible for screening. The
prevalence between the LCSR and the NHIS was compared with prevalence ratios
(PRs) and 95% CIs. Adherence to annual screening was defined as having a
follow-up test within 11 to 15 months of an initial LDCT.
RESULTS: Among 1 159 092 persons who were screened, 90.8% (n = 1 052 591) met
the USPSTF eligibility criteria. Compared with adults from the NHIS who met the
criteria (n = 1257), screening recipients in the LCSR were older (34.7% vs.
44.8% were aged 65 to 74 years; PR, 1.29 [95% CI, 1.20 to 1.39]), more likely to
be female (41.8% vs. 48.1%; PR, 1.15 [CI, 1.08 to 1.23]), and more likely to
currently smoke (52.3% vs. 61.4%; PR, 1.17 [CI, 1.11 to 1.23]). Only 22.3% had a
repeated annual LDCT. If follow-up was extended to 24 months and more than 24
months, 34.3% and 40.3% were adherent, respectively.
LIMITATIONS: Underreporting of LCS and missing data may skew demographic
characteristics of persons reported to be screened. Underreporting of adherence
may result in underestimates of follow-up.
CONCLUSION: Approximately 91% of persons who had LCS met USPSTF eligibility
criteria. In addition to continuing to target all eligible adults, men, those
who formerly smoked, and younger eligible patients may be less likely to be
screened. Adherence to annual follow-up screening was poor, potentially limiting
screening effectiveness.
PRIMARY FUNDING SOURCE: None.
DOI: 10.7326/M22-1325
PMID: 36215712 [Indexed for MEDLINE]
26. J Exp Med. 2022 Nov 7;219(11):e20220504. doi: 10.1084/jem.20220504. Epub 2022
Sep 7.
GPX4 regulates cellular necrosis and host resistance in Mycobacterium
tuberculosis infection.
Amaral EP(1), Foreman TW(2), Namasivayam S(1), Hilligan KL(1), Kauffman KD(2),
Barbosa Bomfim CC(1), Costa DL(3), Barreto-Duarte B(4)(5)(6), Gurgel-Rocha
C(7)(8), Santana MF(9)(10)(11), Cordeiro-Santos M(10)(11)(12), Du Bruyn E(13),
Riou C(13), Aberman K(1), Wilkinson RJ(13)(14)(15), Barber DL(2), Mayer-Barber
KD(16), Andrade BB(4)(5)(6)(17)(18)(19)(20), Sher A(1).
Author information:
(1)Immunobiology Section, Laboratory of Parasitic Diseases, National Institute
of Allergy and Infectious Disease, National Institutes of Health, Bethesda, MD.
(2)T Lymphocyte Biology Section, Laboratory of Parasitic Diseases, National
Institute of Allergy and Infectious Disease, National Institutes of Health,
Bethesda, MD.
(3)Departmento de Bioquímica e Imunologia, Programa de Pós-Graduação em
Imunologia Básica e Aplicada, Faculdade de Medicina de Ribeirão Preto,
Universidade de São Paulo, Ribeirão Preto, Brazil.
…
Cellular necrosis during Mycobacterium tuberculosis (Mtb) infection promotes
both immunopathology and bacterial dissemination. Glutathione peroxidase-4
(Gpx4) is an enzyme that plays a critical role in preventing iron-dependent
lipid peroxidation-mediated cell death (ferroptosis), a process previously
implicated in the necrotic pathology seen in Mtb-infected mice. Here, we
document altered GPX4 expression, glutathione levels, and lipid peroxidation in
patients with active tuberculosis and assess the role of this pathway in mice
genetically deficient in or overexpressing Gpx4. We found that Gpx4-deficient
mice infected with Mtb display substantially increased lung necrosis and
bacterial burdens, while transgenic mice overexpressing the enzyme show
decreased bacterial loads and necrosis. Moreover, Gpx4-deficient macrophages
exhibited enhanced necrosis upon Mtb infection in vitro, an outcome suppressed
by the lipid peroxidation inhibitor, ferrostatin-1. These findings provide
support for the role of ferroptosis in Mtb-induced necrosis and implicate the
Gpx4/GSH axis as a target for host-directed therapy of tuberculosis.
© 2022 Amaral et al.
DOI: 10.1084/jem.20220504
PMCID: PMC9458471
PMID: 36069923 [Indexed for MEDLINE]
27. Nat Chem Biol. 2022 Nov;18(11):1236-1244. doi: 10.1038/s41589-022-01102-7. Epub 2022 Aug 22.
Evybactin is a DNA gyrase inhibitor that selectively kills Mycobacterium
tuberculosis.
Imai Y(#)(1)(2), Hauk G(#)(3), Quigley J(1), Liang L(1), Son S(1), Ghiglieri
M(1), Gates MF(1), Morrissette M(1), Shahsavari N(1), Niles S(1), Baldisseri
D(4), Honrao C(5), Ma X(5), Guo JJ(5)(6), Berger JM(7), Lewis K(8).
Author information:
(1)Antimicrobial Discovery Center, Department of Biology, Northeastern
University, Boston, MA, USA.
(2)Department of Biomolecular Innovation, Institute for Biomedical Sciences,
Shinshu University, Nagano, Japan.
(3)Department of Biophysics and Biophysical Chemistry, Johns Hopkins University
School of Medicine, Baltimore, MD, USA.
(4)Bruker Biospin Corporation, Billerica, MA, USA.
(5)Center for Drug Discovery, Department of Pharmaceutical Sciences,
Northeastern University, Boston, MA, USA.
(6)Barnett Institute for Chemical and Biological Analysis, Department of
Chemistry and Chemical Biology, Northeastern University, Boston, MA, USA.
(7)Department of Biophysics and Biophysical Chemistry, Johns Hopkins University
School of Medicine, Baltimore, MD, USA. jmberger@jhmi.edu.
(8)Antimicrobial Discovery Center, Department of Biology, Northeastern
University, Boston, MA, USA. k.lewis@northeastern.edu.
(#)Contributed equally
The antimicrobial resistance crisis requires the introduction of novel
antibiotics. The use of conventional broad-spectrum compounds selects for
resistance in off-target pathogens and harms the microbiome. This is especially
true for Mycobacterium tuberculosis, where treatment requires a 6-month course
of antibiotics. Here we show that a novel antimicrobial from Photorhabdus
noenieputensis, which we named evybactin, is a potent and selective antibiotic
acting against M. tuberculosis. Evybactin targets DNA gyrase and binds to a site
overlapping with synthetic thiophene poisons. Given the conserved nature of DNA
gyrase, the observed selectivity against M. tuberculosis is puzzling. We found
that evybactin is smuggled into the cell by a promiscuous transporter of
hydrophilic compounds, BacA. Evybactin is the first, but likely not the only,
antimicrobial compound found to employ this unusual mechanism of selectivity.
© 2022. The Author(s), under exclusive licence to Springer Nature America, Inc.
DOI: 10.1038/s41589-022-01102-7
PMID: 35996001 [Indexed for MEDLINE]
28. J Natl Cancer Inst. 2022 Nov 14;114(11):1449-1467. doi: 10.1093/jnci/djac154.
Facilitators and Barriers to Implementation of Lung Cancer Screening: A
Framework-Driven Systematic Review.
Sedani AE(1), Davis OC(2), Clifton SC(3), Campbell JE(1), Chou AF(4).
Author information:
(1)Department of Biostatistics and Epidemiology, Hudson College of Public
Health, University of Oklahoma Health Sciences Center, Oklahoma City, OK, USA.
(2)College of Medicine, University of Oklahoma Health Sciences Center, Oklahoma
City, OK, USA.
(3)Robert M. Bird Health Sciences Library, University of Oklahoma Health
Sciences Center, Oklahoma City, OK, USA.
(4)Department of Family and Preventive Medicine, College of Medicine, University
of Oklahoma Health Sciences Center, Oklahoma City, OK, USA.
BACKGROUND: The purpose of this study is to undertake a comprehensive systematic
review to describe multilevel factors (barriers and facilitators) that may
influence the implementation of low-dose chest computed tomography for lung
cancer screening in the United States.
METHODS: Systematic literature searches were performed using 6 online databases
and citation indexes for peer-reviewed studies, for articles published from 2013
to 2021. Studies were classified into 3 perspectives, based on the study's unit
of analysis: system, health-care provider, and patient. Barriers and
facilitators identified for each study included in our final review were then
coded and categorized using the Consolidate Framework for Implementation
Research domains.
RESULTS: At the system level, the 2 most common constructs were external policy
and incentives and executing the implementation process. At the provider level,
the most common constructs were evidence strength and quality of the
intervention characteristics, patient needs and resources, implementation
climate, and an individual's knowledge and beliefs about the intervention. At
the patient level, the most common constructs were patient needs and resources,
individual's knowledge and beliefs about the intervention, and engaging in the
implementation process. These constructs can act as facilitators or barriers to
lung cancer screening implementation.
CONCLUSIONS: Applying the Consolidate Framework for Implementation Research
domains and constructs to understand and specify factors facilitating uptake of
lung cancer screening as well as cataloging the lessons learned from previous
efforts helps inform the development and implementation processes of lung cancer
screening programs in the community setting.
REGISTRATION: PROSPERO, CRD42021247677.
© The Author(s) 2022. Published by Oxford University Press.
DOI: 10.1093/jnci/djac154
PMCID: PMC9664175
PMID: 35993616 [Indexed for MEDLINE]
29. J Clin Oncol. 2022 Nov 1;40(31):3587-3592. doi: 10.1200/JCO.21.02911. Epub 2022 Aug 12.
Updated Analysis of NEJ009: Gefitinib-Alone Versus Gefitinib Plus Chemotherapy
for Non-Small-Cell Lung Cancer With Mutated EGFR.
Miyauchi E(1), Morita S(2), Nakamura A(3), Hosomi Y(4), Watanabe K(5), Ikeda
S(6), Seike M(7), Fujita Y(8), Minato K(9), Ko R(10), Harada T(11), Hagiwara
K(12), Kobayashi K(13), Nukiwa T(14), Inoue A(15); North-East Japan Study Group.
Author information:
(1)Department of Respiratory Medicine, Tohoku University Hospital, Sendai,
Japan.
(2)Department of Biomedical Statistics and Bioinformatics, Kyoto University
Graduate School of Medicine, Kyoto, Japan.
(3)Department of Respiratory Medicine, Sendai Kosei Hospital, Sendai, Japan.
…
Clinical trials frequently include multiple end points that mature at different
times. The initial report, typically based on the primary end point, may be
published when key planned coprimary or secondary analyses are not yet
available. Clinical Trial Updates provide an opportunity to disseminate
additional results from studies, published in JCO or elsewhere, for which the
primary end point has already been reported.In a randomized, open-label, phase
III NEJ009 study, gefitinib plus chemotherapy significantly improved
progression-free survival (PFS) and overall survival (OS) compared with
gefitinib-alone in patients with untreated non-small-cell lung cancer harboring
mutations in epidermal growth factor receptor. Herein, we report the updated
survival outcome and long-term tolerability. Patients were randomly assigned to
gefitinib (gefitinib 250 mg orally, once daily) and gefitinib combined with
carboplatin plus pemetrexed (GCP in a 3-week cycle for six cycles followed by
concurrent gefitinib and pemetrexed maintenance) groups. At the data cutoff (May
22, 2020), GCP demonstrated significantly better PFS2 (hazard ratio, 0.77; 95%
CI, 0.62 to 0.97; P = .027) than gefitinib. However, the updated median OS was
38.5 months (95% CI, 31.1 to 47.1) and 49.0 months (95% CI, 41.8 to 56.7) in the
gefitinib and GCP groups, respectively (hazard ratio, 0.82; 95% CI, 0.64 to
1.06; P = .127). The OS in both groups was similar for the overall patient
population. No severe adverse events occurred since the first report. This
updated analysis revealed that the GCP regimen improved PFS and PFS2 with an
acceptable safety profile compared with gefitinib-alone. GCP is more efficient
than gefitinib monotherapy as a first-line treatment for non-small-cell lung
cancer with epidermal growth factor receptor mutations.
DOI: 10.1200/JCO.21.02911
PMCID: PMC9622660
PMID: 35960896 [Indexed for MEDLINE]
30. Lancet Infect Dis. 2022 Nov;22(11):1617-1625. doi:
10.1016/S1473-3099(22)00425-X. Epub 2022 Aug 4.
Nationwide tuberculosis outbreak in the USA linked to a bone graft product: an
outbreak report.
Schwartz NG(1), Hernandez-Romieu AC(2), Annambhotla P(3), Filardo TD(4),
Althomsons SP(5), Free RJ(3), Li R(2), Wyatt Wilson W(2), Deutsch-Feldman M(4),
Drees M(6), Hanlin E(7), White K(8), Lehman KA(9), Thacker TC(9), Brubaker
SA(10), Clark B(10), Basavaraju SV(3), Benowitz I(3), Burton Glowicz J(3), Cowan
LS(5), Starks AM(5), Bamrah Morris S(5), LoBue P(5), Stewart RJ(5), Wortham
JM(5), Haddad MB(5); Bone Allograft Tuberculosis Investigators.
Author information:
(1)Division of Tuberculosis Elimination, National Center for HIV, Viral
Hepatitis, STD, and TB Prevention, US Centers for Disease Control and
Prevention, Atlanta, GA, USA; Epidemic Intelligence Service, US Centers for
Disease Control and Prevention, Atlanta, GA, USA. Electronic address:
nschwartz@cdc.gov.
(2)Epidemic Intelligence Service, US Centers for Disease Control and Prevention,
Atlanta, GA, USA; Division of Healthcare Quality Promotion, National Center for
Emerging and Zoonotic Infectious Diseases, US Centers for Disease Control and
Prevention, Atlanta, GA, USA.
(3)Division of Healthcare Quality Promotion, National Center for Emerging and
Zoonotic Infectious Diseases, US Centers for Disease Control and Prevention,
Atlanta, GA, USA.
…
Comment in
Lancet Infect Dis. 2022 Nov;22(11):1522-1523.
BACKGROUND: Mycobacterium tuberculosis transmission through solid organ
transplantation has been well described, but transmission through transplanted
tissues is rare. We investigated a tuberculosis outbreak in the USA linked to a
bone graft product containing live cells derived from a single deceased donor.
METHODS: In this outbreak report, we describe the management and severity of the
outbreak and identify opportunities to improve tissue transplant safety in the
USA. During early June, 2021, the US Centers for Disease Control and Prevention
(CDC) worked with state and local health departments and health-care facilities
to locate and sequester unused units from the recalled lot and notify, evaluate,
and treat all identified product recipients. Investigators from CDC and the US
Food and Drug Administration (FDA) reviewed donor screening and tissue
processing. Unused product units from the recalled and other donor lots were
tested for the presence of M tuberculosis using real-time PCR (rt PCR) assays
and culture. M tuberculosis isolates from unused product and recipients were
compared using phylogenetic analysis.
FINDINGS: The tissue donor (a man aged 80 years) had unrecognised risk factors,
symptoms, and signs consistent with tuberculosis. Bone was procured from the
deceased donor and processed into 154 units of bone allograft product containing
live cells, which were distributed to 37 hospitals and ambulatory surgical
centres in 20 US states between March 1 and April 2, 2021. From March 3 to June
1, 2021, 136 (88%) units were implanted into 113 recipients aged 24-87 years in
18 states (some individuals received multiple units). The remaining 18 units
(12%) were located and sequestered. 87 (77%) of 113 identified product
recipients had microbiological or imaging evidence of tuberculosis disease.
Eight product recipients died 8-99 days after product implantation (three deaths
were attributed to tuberculosis after recognition of the outbreak). All 105
living recipients started treatment for tuberculosis disease at a median of 69
days (IQR 56-81) after product implantation. M tuberculosis was detected in all
eight sequestered unused units tested from the recalled donor lot, but not in
lots from other donors. M tuberculosis isolates from unused product and
recipients were more than 99·99% genetically identical.
INTERPRETATION: Donor-derived transmission of M tuberculosis via bone allograft
resulted in substantial morbidity and mortality. All prospective tissue and
organ donors should be routinely assessed for tuberculosis risk factors and
clinical findings. When these are present, laboratory testing for M tuberculosis
should be strongly considered.
FUNDING: None.
Copyright © 2022 Elsevier Ltd. All rights reserved.
DOI: 10.1016/S1473-3099(22)00425-X
PMCID: PMC9605268
PMID: 35934016 [Indexed for MEDLINE]
31. J Clin Oncol. 2022 Nov 20;40(33):3808-3816. doi: 10.1200/JCO.21.02986. Epub 2022 Jun 27.
Antibody Response to COVID-19 mRNA Vaccine in Patients With Lung Cancer After
Primary Immunization and Booster: Reactivity to the SARS-CoV-2 WT Virus and
Omicron Variant.
Valanparambil RM(1)(2), Carlisle J(3), Linderman SL(1)(2), Akthar A(1)(2),
Millett RL(3), Lai L(1)(4)(5), Chang A(1)(2)(3)(6), McCook-Veal AA(7),
…
Author information:
(1)Emory Vaccine Center, Emory University School of Medicine, Atlanta, GA.
(2)Department of Microbiology and Immunology, Emory University, Atlanta, GA.
(3)Winship Cancer Institute, Atlanta, GA.
…
Update of
medRxiv. 2022 Jan 23;:
PURPOSE: To examine COVID-19 mRNA vaccine-induced binding and neutralizing
antibody responses in patients with non-small-cell lung cancer (NSCLC) to
SARS-CoV-2 614D (wild type [WT]) strain and variants of concern after the
primary 2-dose and booster vaccination.
METHODS: Eighty-two patients with NSCLC and 53 healthy volunteers who received
SARS-CoV-2 mRNA vaccines were included in the study. Blood was collected
longitudinally, and SARS-CoV-2-specific binding and neutralizing antibody
responses were evaluated by Meso Scale Discovery assay and live virus Focus
Reduction Neutralization Assay, respectively.
RESULTS: A majority of patients with NSCLC generated binding and neutralizing
antibody titers comparable with the healthy vaccinees after mRNA vaccination,
but a subset of patients with NSCLC (25%) made poor responses, resulting in
overall lower (six- to seven-fold) titers compared with the healthy cohort (P =
< .0001). Although patients age > 70 years had lower immunoglobulin G titers (P
= < .01), patients receiving programmed death-1 monotherapy, chemotherapy, or a
combination of both did not have a significant impact on the antibody response.
Neutralizing antibody titers to the B.1.617.2 (Delta), B.1.351 (Beta), and in
particular, B.1.1.529 (Omicron) variants were significantly lower (P = < .0001)
compared with the 614D (WT) strain. Booster vaccination led to a significant
increase (P = .0001) in the binding and neutralizing antibody titers to the WT
and Omicron variant. However, 2-4 months after the booster, we observed a five-
to seven-fold decrease in neutralizing titers to WT and Omicron viruses.
CONCLUSION: A subset of patients with NSCLC responded poorly to the SARS-CoV-2
mRNA vaccination and had low neutralizing antibodies to the B.1.1.529 Omicron
variant. Booster vaccination increased binding and neutralizing antibody titers
to Omicron, but antibody titers declined after 3 months. These data highlight
the concern for patients with cancer given the rapid spread of SARS-CoV-2
Omicron variant.
DOI: 10.1200/JCO.21.02986
PMCID: PMC9671759
PMID: 35759727 [Indexed for MEDLINE]
32. Am J Respir Crit Care Med. 2022 Nov 1;206(9):1153-1162. doi:
10.1164/rccm.202201-0114OC.
Solid Fuel, Secondhand Smoke, and Lung Cancer Mortality: A Prospective Cohort of
323,794 Chinese Never-Smokers.
Cheng ES(1)(2), Chan KH(3)(4), Weber M(2), Steinberg J(2), Young J(1)(2),
Canfell K(2)(5), Yu XQ(2).
Author information:
(1)Sydney School of Public Health and.
(2)the Daffodil Centre, the University of Sydney, Sydney, New South Wales,
Australia.
(3)Oxford British Heart Foundation Centre of Research Excellence and.
(4)Clinical Trial Service Unit and Epidemiological Studies Unit, Nuffield
Department of Population Health, University of Oxford, Oxford, United Kingdom;
and.
(5)Prince of Wales Clinical School, University of New South Wales, Sydney, New
South Wales, Australia.
Comment in
Am J Respir Crit Care Med. 2022 Nov 1;206(9):1065-1067.
Rationale: Household air pollution and secondhand tobacco smoke are known
carcinogens for lung cancer, but large-scale estimates of the relationship with
lung cancer mortality are lacking. Objectives: Using the large-scale cohort
China Kadoorie Biobank, we prospectively investigated associations between these
two risk factors and lung cancer death among never-smokers. Methods: The Biobank
recruited 512,715 adults aged 30-79 years from 10 regions in China during
2004-2008. Self-reported never-smoking participants were followed up to December
31, 2016, with linkage to mortality data. Total duration of exposure to
household air pollution was calculated from self-reported domestic solid fuel
use. Exposure to secondhand tobacco smoke was ascertained using exposure at home
and/or other places. Hazard ratios and 95% confidence intervals for associations
between these two exposures and lung cancer death were estimated using Cox
regression, adjusting for key confounders. Measurements and Main Results: There
were 979 lung cancer deaths among 323,794 never-smoking participants without a
previous cancer diagnosis during 10.2 years of follow-up. There was a log-linear
positive association between exposure to household air pollution and lung cancer
death, with a 4% increased risk per 5-year increment of exposure (hazard
ratio = 1.04; 95% confidence interval = 1.01-1.06; P trend = 0.0034), and
participants with 40.1-50.0 years of exposure had the highest risk compared with
the never-exposed (hazard ratio = 1.53; 95% confidence interval = 1.13-2.07).
The association was largely consistent across various subgroups. No significant
association was found between secondhand smoke and lung cancer death.
Conclusions: This cohort study provides new prospective evidence suggesting that
domestic solid fuel use is associated with lung cancer death among
never-smokers.
DOI: 10.1164/rccm.202201-0114OC
PMCID: PMC9704832
PMID: 35616543 [Indexed for MEDLINE]
33. J Clin Oncol. 2022 Nov 1;40(31):3593-3602. doi: 10.1200/JCO.21.02278. Epub 2022 May 23.
Post Hoc Analysis of Lorlatinib Intracranial Efficacy and Safety in Patients
With ALK-Positive Advanced Non-Small-Cell Lung Cancer From the Phase III CROWN
Study.
Solomon BJ(1), Bauer TM(2), Ignatius Ou SH(3), Liu G(4), Hayashi H(5), Bearz
A(6), Penkov K(7), Wu YL(8), Arrieta O(9), Jassem J(10), Calella AM(11), Peltz
G(12), Polli A(11), Thurm H(13), Mok T(14).
Author information:
(1)Peter MacCallum Cancer Centre, Melbourne, VIC, Australia.
(2)Sarah Cannon Research Institute/Tennessee Oncology, PLLC, Nashville, TN.
(3)University of California Irvine School of Medicine, Orange, CA.
…
Comment in
J Clin Oncol. 2022 Nov 1;40(31):3564-3568.
PURPOSE: Lorlatinib significantly improved progression-free survival (PFS)
versus crizotinib and showed robust intracranial activity in patients with
previously untreated advanced ALK-positive non-small-cell lung cancer (NSCLC) in
the phase III CROWN trial. Here, we report post hoc efficacy outcomes in
patients with and without brain metastases at baseline, and present data on the
incidence and management of CNS adverse events (AEs) in CROWN.
METHODS: Eligible patients were randomly assigned 1:1 to first-line lorlatinib
(100 mg once daily) or crizotinib (250 mg twice a day); no crossover between
treatment arms was permitted. Tumor assessments, including CNS magnetic
resonance imaging, were performed at screening and then at 8-week intervals.
Regular assessments of patient-reported outcomes were conducted.
RESULTS: PFS by blinded independent central review was improved with lorlatinib
versus crizotinib in patients with and without brain metastases at baseline
(12-month PFS rates: 78% v 22% and 78% v 45%, respectively). Lorlatinib was
associated with lower 12-month cumulative incidence of CNS progression versus
crizotinib in patients with (7% v 72%) and without (1% v 18%) brain metastases
at baseline. In total, 35% of patients had CNS AEs with lorlatinib, most of
grade 1 severity. Occurrence of CNS AEs did not result in a clinically
meaningful difference in patient-reported quality of life. At analysis, 56% of
CNS AEs had resolved (33% without intervention; 17% with lorlatinib dose
modification), and 38% were unresolved; most required no intervention.
Lorlatinib dose modification did not notably influence PFS.
CONCLUSION: First-line lorlatinib improved PFS outcomes and reduced CNS
progression versus crizotinib in patients with advanced ALK-positive
non-small-cell lung cancer with or without brain metastases at baseline. Half of
all CNS AEs resolved without intervention or with lorlatinib dose modification.
DOI: 10.1200/JCO.21.02278
PMCID: PMC9622589
PMID: 35605188 [Indexed for MEDLINE]





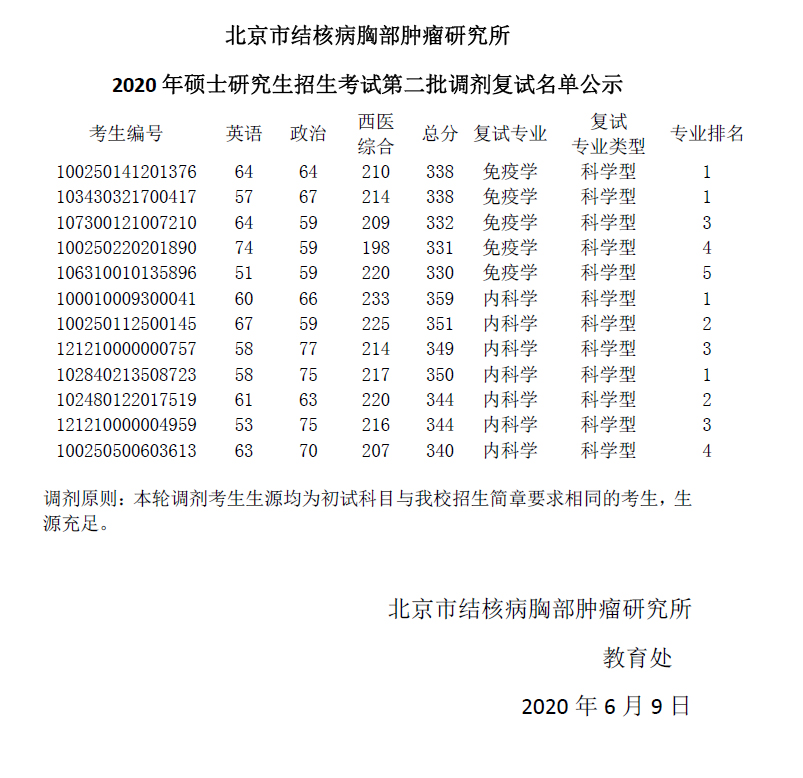


.jpg)











